Drug information
Clesrovimab
Not provided
Biotherapeutic
Clesrovimab (MK-1654) is an investigational human IgG1 monoclonal antibody (mAb) currently in clinical development for the prevention of Respiratory syncytial virus (RSV). It is being studied as protection against mild, moderate, and severe RSV in preterm, full-term, and at-risk infants during their first RSV season. Clesrovimab is designed to be administered at the same single-dose irrespective of birth weight and exhibits potent in vitro neutralization of RSV-A and RSV-B clinical isolates via high affinity binding to the RSV fusion (F) protein antigenic site IV. Engineered YTE substitution mutations in the mAb fragment crystallizable (Fc) domain result in an extended half-life through enhanced neonatal Fc receptor binding, with a reported half-life in adults ranging from 73 to 88 days.
The U.S. Food and Drug Administration (FDA) has accepted the Biologics License Application (BLA) for clesrovimab (MK-1654), Merck's investigational prophylactic long-acting monoclonal antibody designed to protect infants from respiratory syncytial virus (RSV) disease during their first RSV season. The FDA has set a Prescription Drug User Fee Act (PDUFA), or target action, date of June 10, 2025.
Unknown
Therapeutic area(s)
- Respiratory syncytial virus (RSV)
- Prevention
Administration route
Intramuscular
Associated long-acting platforms
Monoclonal antibodies and antibody drug conjugates
Use of drug
- Administered by a nurse
- Administered by a specialty health worker
- Administered by a community health worker
Not provided
Dosage
100 mg in 0.5 mL
Not provided
Not provided
Not provided
Not provided
Not provided
Associated technologies
Not provided
Comment & Information
Developer(s)

Merck & Co., Inc. is an American multinational pharmaceutical company known as Merck Sharp & Drone (MSD) in territories outside of the USA and Canada. Merck was originally established in 1891, and is headquartered in Rahway, New Jersey. The company is particularly well known for developing and manufacturing biologic therapies, vaccines, medicines and animal health products.
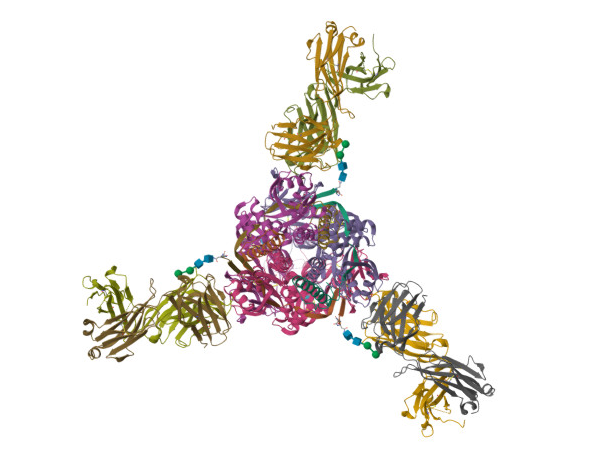
Drug structure
Scale-up and manufacturing prospects
General manufacturing requirements and production scale-up for therapeutic monoclonal antibody (mAb) products is primarily focused on pharmacokinetic suitability, formulation stability and the overall maintenance of product quality. Industrial bioprocessing steps can also potentially introduce additional challenges regarding mAb formulation viscosity and aggregation propensity.
Industrial bioreactor vessel with a production volume capacity of between 5-25kL. Continuous disc stack centrifuges for bioreactor harvesting with subsequent membrane and depth filtration for supernatant clarification. Recombinant protein-A chromatography or other suitable affinity capture apparatus followed by two chromatographic polishing steps such as cation- and anion-exchange. Ultrafiltration membrane system to concentrate and formulate the final product.
MAbs are highly dependent on their structural, chemical and conformational stability for biological activity. Chemical degradation of mAbs during manufacture can lead to the generation of product variants and complex impurity profiles resulting from a wide range of processes, including: N-linked glycosylation, isomerisation, fragmentation, deamidation, oxidation and C-terminal lysine clipping. Additionally prior to packaging, the final product requires close monitoring for the presence of residual contaminants such as endotoxins and pro-inflammatory peptidoglycans.
Formulation characterisation steps for therapeutic mAb products include (but are not limited to): (1) Identification of post-translational modifications using ion-exchange chromatography and capillary isoelectric focusing, (2) Measurement of concentration dependent aggregation rates via thermal differential scanning calorimetry, sub-visible particle quantitation and size-exclusion chromatography, and (3) Antibody clipping and fragmentation detection by capillary electrophoresis.
Excipients
No proprietary excipient used
No novel excipient or existing excipient used
No residual solvent used
Delivery device(s)
No delivery device
Publications
Phuah JY, Maas BM, Tang A, Zhang Y, Caro L, Railkar RA, Swanson MD, Cao Y, Li H, Roadcap B, Catchpole AP, Aliprantis AO, Vora KA. Quantification of clesrovimab, an investigational, half-life extended, anti-respiratory syncytial virus protein F human monoclonal antibody in the nasal epithelial lining fluid of healthy adults. Biomed Pharmacother. 2023 Dec 31;169:115851. DOI: 10.1016/j.biopha.2023.115851. Epub 2023 Nov 14. PMID: 37976891.
Background: Clesrovimab (MK-1654) is an investigational, half-life extended human monoclonal antibody (mAb) against RSV F glycoprotein in clinical trials as a prophylactic agent against RSV infection for infants.
Methods: This adult study measured clesrovimab concentrations in the serum and nasal epithelial lining fluid (ELF) to establish the partitioning of the antibody after dosing. Clesrovimab concentrations in the nasal ELF were normalized for sampling dilution using urea concentrations from ELF and serum. Furthermore, in vitro RSV neutralization of human nasal ELF following dosing was also measured to examine the activity of clesrovimab in the nasal compartment.
Findings: mAbs with YTE mutations are reported in literature to partition ∼1-2 % of serum antibodies into nasal mucosa. Nasal: serum ratios of 1:69-1:30 were observed for clesrovimab in two separate adult human trials after urea normalization, translating to 1.4-3.3 % of serum concentrations. The nasal PK and estimates of peripheral volume of distribution correlated with higher extravascular distribution of clesrovimab. These higher concentration of the antibody in the nasal ELF corroborated with the nasal sample's ability to neutralize RSV ex vivo. An overall trend of decreased viral plaque AUC was also noted with increasing availability of clesrovimab in the nasal ELF from a human RSV challenge study.
Interpretation: Along with its extended half-life, the higher penetration of clesrovimab into the nasal epithelial lining fluid and the associated local increase in RSV neutralization activity could offer infants better protection against RSV infection.
Keywords: Monoclonal antibody; Nasal epithelial lining fluid; RSV; Respiratory syncytial virus; Urea normalization.
Additional documents
No documents were uploaded
Collaborate for development
Consider on a case by case basis, collaborating on developing long acting products with potential significant public health impact, especially for low- and middle-income countries (LMICs), utilising the referred to long-acting technology
Share technical information for match-making assessment
Provide necessary technical information to a potential partner, under confidentiality agreement, to enable preliminary assessment of whether specific medicines of public health importance in LMICs might be compatible with the referred to long-acting technology to achieve a public health benefit
Work with MPP to expand access in LMICs
In the event that a product using the referred to long-acting technology is successfully developed, the technology IP holder(s) will work with the Medicines Patent Pool towards putting in place the most appropriate strategy for timely and affordable access in low and middle-income countries, including through licensing